-
About
- Leadership & Faculty
- News & Events
-
Admissions
-
Academics
- Graduate
- Advanced Clinical Training
- Continuing Education
- Academic Departments
- Academic Offices
- Simulation Experiences
-
Student Life
- Offices
-
Research
-
- Transformative Research
- Centers & Shared Resources
-
-
Hospitals & Clinics
- Emergency Care
- Hospital Services
-
Community Outreach
- Volunteer
Surgical Management of Impinging or Overriding Dorsal Spinous Processes
José M. García-López, VMD, DACVS, DACVSMR I. INTRODUCTION Dorsal spinous process (DSP) impingement or overriding (ORDSP), often referred as “kissing ...

José M. García-López, VMD, DACVS, DACVSMR
I. INTRODUCTION
Dorsal spinous process (DSP) impingement or overriding (ORDSP), often referred as “kissing spines”, has been reported as the most common cause of back pain in the horse.1 Impingement of the DSPs is found mostly at the level of T13- T18, but it can also affect the lumbar DSPs.1 Factors historically associated to this condition include poor conformation, poor conditioning, rider-horse mismatch and chronic use of an ill- fitted saddle. Clinical signs may include a vague history of poor performance, change in head/neck carriage, unwillingness to move in a certain direction, concurrent hindlimb lameness, unwillingness to bend, and pain of varying degrees of intensity upon firm palpation of the affected region.1
Diagnosis of active ORDSP can be challenging at times since radiography alone does not tell us the amount of current inflammation present, and the presence of bony remodeling, impingement and/or overriding does not mean that the horse is suffering from this condition, as radiographic signs of ORDSP have been reported in clinically normal horses. Townsend and colleagues (1986) reported of the presence of ORDSP during post mortem examination in 83% of 23 horses with functionally normal thoracolumbar spines.2 There are a number of radiographic grading scales used by clinicians in order to classify the degree of ORDSP, the two most commonly used are those described by Pettersson and colleagues and by Dyson and Denoix, using a 1-3 (Grade 1- narrowing of 2 or more interspinous spaces with narrowing; Grade 2- impingement between 2 or more dorsal spinous processes with sclerotic and/or radiolucent areas; Grade 3- impingement and overriding of 2 or more dorsal spinous processes with sclerosis and/or radiolucent areas) and 1-4 grading scale (Grade 1- narrowing of the interspinous with mild increased opacity of the cortical margins of the dorsal spinous processes [Fig. 1]; Grade 2- loss of in the interspinous space with moderate increased opacity of the cortical margins of the dorsal spinous processes [Fig. 2]; Grade 3- severe increased opacity of the cortical margins of the dorsal spinous processes [Fig. 3]; Grade 4- severe increased opacity of the cortical margins, osteolysis, change in shape and overriding of the dorsal spinous processes [Fig. 4]), respectively.3,4
In order to try to better correlate any radiographic findings (of ORDSP) with its potential role clinically as well as to provide certain degree of “objectivity”, the use of nuclear scintigraphy of this region, together with the physical examination findings and lameness workup, can be a critical imaging tool. However, it is important to point out that the presence of increased radioisotope uptake is not synonymous with back pain.5
II. TREATMENT FOR ORDSP
Conservative/Medical:Historically, medical management has consisted of local injections anti-inflammatories, physiotherapy, mesotherapy and/or focused extracorporeal shockwave therapy (ESWT). Although medical management can be highly successful, it is important to communicate with owners and trainers the very likely need for repeated treatment, ideally every 6-12 months. In a recent study, Coomer and colleagues reported an 89% short term improvement in the clinical signs of 38 horses suffering from ORDSP treated medically by means of local injections with anti-inflammatories, with a return of back pain in 56% of the horses a median of 75 days (range 12-334 days).6
Conservative management by the way of rest alone can be helpful in some cases. The aim of rest in horses suffering from ORDSP is to reduce inflammation associated with the bone contact, bony remodeling and soft tissue damage.1 However, in order to effectively reduce inflammation, rest has to be long enough to be beneficial, typically 3-9 months. This is in part (other reasons include loss of muscle mass and strength) why rest is typically combined with some kind of medical therapy or is not necessarily this author’s first treatment choice.
Medication of the affected interspinous spaces is one of the most commonly used medical treatment modalities, consisting of injecting a combination of anti-inflammatories and analgesics such as Depo-Medrol (40-100 mg/space), Sarapin (10-15 ml), and 5-7 ml of carbocaine. Care should be taken with regards to drug withdrawal for horses that are in active competition as this can be highly variable among different organizations.
Treatment of the affected DSPs with a course of focused ESWT consisting of anywhere from one treatment (for cases with only bony inflammation) to 3-4 treatments (for those with bony and ligamentous injuries). This author performs ESWT treatments generally spaced approximately 2-3 weeks apart. Although the exact mechanism of ESWT action is not completely understood, its analgesic properties and proposed microtrauma effect appear to provide an environment conducive to healing.1 Following treatment with either interspinous injections or ESWT, these horses will be rested for a variable amount of time (1-6 weeks) except for those with ligamentous injuries where follow-up ultrasound examinations are performed every 6 weeks until deemed appropriate to resume exercise. Once back into exercise they are typically worked on a lunge line before re-introducing them to work under saddle.
Coudry and colleagues (2007) demonstrated the efficacy of tiludronatea with regards to the improvement of dorsal flexibility in horses suffering from OA of the vertebral column.7 Although this condition is different than DSP impingement and inflammation, there is the suspicion that some of these horses are also suffering from similar changes at the level of the vertebral column, which has prompted a more careful evaluation of this area in addition to the DSPs. The reported treatment protocol is 10 vials (500 mg total; 1 mg/kg) diluted in 500 ml – 1L of Lactated ringer’s solution (LRS) given IV with a second treatment 2-3 months later. Pre-treatment with flunixon meglumineb (500 mg IV) is routinely recommended in order to decrease the chances of colic signs occasionally associated with the acute administration of tiludronate.a It is recommended to perform a complete chemistry panel prior to administration of any bisphosphonate in order to assess renal status of the patient.
Another treatment that has been used to manage back pain with increased frequency during the past couple of years is mesotherapy. Mesotherapy relies on the concept of inhibition of nerves carrying painful information from the deep structures within a spinal segment by stimulation of nerves from more superficial structures.1 Mesotherapy consists of a series of rows of intradermal injections of corticosteroids, sarapin, carbocaine and/or saline placed at the level and caudal to the source of the pain.
Surgical Management: Historically, horses that do not respond to medical management or those suffering from severe ORDSP would be reasonable candidates to be managed surgically. Until recently, surgical options consisted of partial removal of the affected DSPs, either through a midline or paramedian incision either under general anesthesia or standing, or using an endoscopic approach via small incisions also under general anesthesia.8-11 All of these procedures although highly effective, are either costly, have long recuperation times or suffer from a relative number of incisional complications. Walmsley and colleagues (2002) reported on their experience managing 215 horses suffering from ORDSP by removal of every other affected DSPs.8 Their results showed 81% returned to athletic use with 72% of the cases returning to full work. A total of 13 horses (16.5%) exhibited incisional complications or infections which resolved but not without further intervention. It has been the author’s experience that horses managed in this fashion are able to return to light work anywhere between 3 and 6 months. A similar procedure where sections of the affected DSPs are resected but with the horse standing under light sedation has also been reported.9 This technique has the advantage of avoiding general anesthesia; however, it can suffer from an increase in incisional complications. In 2007, Desbrosse and colleagues described a new technique whereby the resection of the affected DSPs was performed under general anesthesia but using a modified endoscope in a minimally invasive manner.10 This technique showed a lot of promise with a similar positive outcome and no reported incisional complications but has failed to gain major popularity due to the need for extra cost and specialized instrumentation.
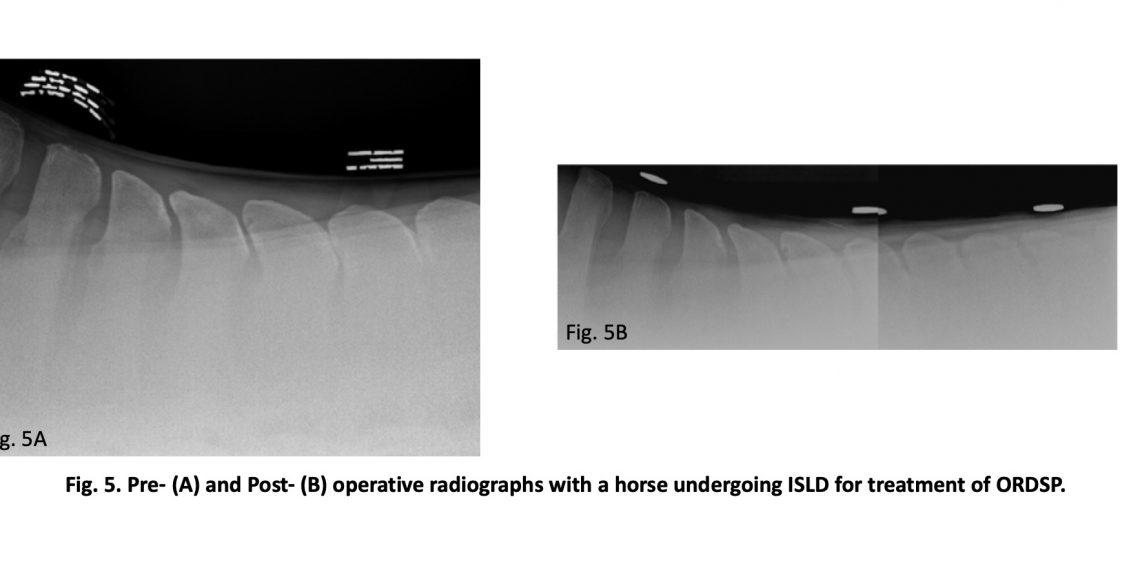
In 2012, Coomer and colleagues described a new, minimally invasive technique which is performed with the horse standing under mild sedation and local anesthesia which, based on their reported success, has changed the way that some clinicians tackle horses suffering from ORDSP.6 Their technique, Interspinous ligament desmotomy (ISLD), consists of making a 1-cm paramedian incision on the left epaxial region, just lateral to the supraspinous ligament (SSL) through which a large curved may scissor is inserted. Using a combination of radiographic control and needle placement prior to and during the entire surgery, the affected spaces are identified and properly marked. Using blunt dissection of the thoracolumbar fascia, a “tunnel” is made immediately ventral to the SSL but dorsal to the ISL, in between the affected DSPs. Once this tunnel is created, the scissors are rotated 90° so they are in a parallel alignment with the interspinous space. The ligament is then transected for a distance of up to 6 cm. The purpose of the transection of the ligament has 2 purposes: (1) to allow an increase in the interspinous space (effectively stopping the ORDSP or “kissing”; Fig. 5), and (2) to relieve the tension on afferent nociceptive receptors located at the level of the insertion of the ISL, thus abolishing the sensation of pain.6 Following the procedure, these horses undergo an 8-week rehabilitation program consisting of stall rest with hand- walking exercise for the first month followed by another 4 weeks of limited turnout in a small paddock with lunging exercise using a Pessoa. In addition, strengthening and spinal mobilization exercises such as carrot stretches, and belly pushes are strongly recommended starting 5 days following the ISLD. Coomer and colleagues (2012) reported on their short- and long-term results using this technique on 35 horses diagnosed with ORDSP.6 Their results showed that 95% of the horses treated by means of ISLD had a resolution of the signs of back pain and were able to return to ridden work. After following these cases over a year post-op, none showed a recurrence of back pain although 46% of them (n=16) developed other lameness problems. All but 3 of these cases were able to be managed medically and resumed athletic exercise, either at their normal level of athletic activity (n=10) or at a reduced level (n=3). The 3 horses that did not have sufficient resolution of the lameness were retired.6 There appeared to be no correlation between the ISLD procedure and the occurrence of the lameness.
ORDSP continues to be a very challenging condition affecting the equine athlete. As clinicians, we need to continue to improve in our evaluation of these cases in order to obtain an accurate diagnosis and have a better understanding of the structures involved in these cases. In addition, we need to recognize the effects of back pain with regards to its influence on fore- or hind- limb lameness. The advent of ISLD as an apparently safe, minimally invasive and relatively inexpensive procedure might allow us to manage these cases in an effective manner when combined with the appropriate rehabilitation and strengthening program.
ACKNOWLEDGMENTS
Declaration of Ethics:The author has adhered to the Principles of Veterinary Medical Ethics as stipulated by the AVMA.
Conflicts of Interest:The author has no conflict of interest.
REFERENCES AND FOOTNOTES
- Henson FM, Kidd JA. Overriding dorsal spinous processes. In: Henson FM, ed. Equine Back Pathology. Oxford: Blackwell Publishing, 2009; 147– 156.
- Townsend HGG, Leach DH, Doige CE, et al. Relationship between spinal biomechanics and pathological changes in the equine thoracolumbar spine. Equine Vet J 1986;18:107-112.
- Pettersson H, Strömberg B, Myrin I. Das thorkolumbale, interspinale Syndrom (TLI) des Reitpferdes – Retriospektiver Vergleich konservativ und chirurgisch behandelter Fälle. Pferdeheilkunde 1987;3:313-319.
- Denoix JM, Dyson Thoracolumbar Spine. In: Ross MW and Dyson SJ, eds. Diagnosis and Management of Lameness in the Horse, 2nd ed. St. Louis, Elsevier, 2011;592-605.
- Zimmerman M, Dyson S, Murray Close, Impinging and overriding spinous processes in the thoracolumbar spine: the relationship between radiological and scintigraphic findings and clinical signs. Equine Vet J 2012;44:178-184.
- Coomer RPC, McKane SA, Smith N, et al. A controlled study evaluating a novel surgical treatment for kissing spines in standing sedated horses. Vet Surg 2012;41:890-897.
- Coudry V, Thibaud D, Riccio B, et al. Efficacy of tiludronate in the treatment of horses with signs of pain associated with osteoarthritic lesions of the thoracolumbar vertebral column. Am J Vet Res 2007;68:329–337.
- Walmsley JP, Pettersson H, Winberg F, et al. Impingement of the dorsal spinous processes in two hundred and fifteen horses: case selection, surgical technique and results. Equine Vet J 2002;34:23-28.
- Perkins JD, Schumacher J, Kelly G, et al. Subtotal ostectomy of dorsal spinous processes performed in nine standing horses. Vet Surg 2005;34:625–629.
- Desbrosse FG, Perrin R, Launois T, et al. Endoscopic resection of dorsal spinous processes and interspinous ligament in ten horses. Vet Surg 2007;36:149–155.
- Jacklin BD, Minshall GJ, Wright A new technique for subtotal (cranial wedge) ostectomy in the treatment of impinging/overriding spinous processes: description of technique and outcome of 25 cases. Equine Vet J 2012;44:136-142.
- Tildren®, CEVA, Santé Animale, Banamine
- Merck Animal Health, Intervet, Inc. Madison, NJ
This paper was presented at the 2018 AAEP 360° Back Pain and Pelvic Dysfunction course.